Has the USA Sterilized 2+% of all 6-17 year olds?
Between 1.83% and 7.95% of the USA's 6-17 year olds have received gender medicine treatments. A majority of them are expected to be sterilized. This population is projected to continue to grow significantly.
Note: This article was published under 4W's "self publishing" program, did not go through 4W's editorial process, and does not necessarily represent the views of 4W or its staff.
Update 1/19/2024: The information needed to perform the calculations that I said needed to be conducted was recently published. This update revises the estimates of the original article downward to 20% of the original lower boundary calculation. Important details that are consistent: (1) insurance "creative coding" and uninsured medical care dominates the market, so the assumption that Respaut and Terhune (2022) actually measured this effect as opposed to the full population holds; (2) the rate of sterilization for those receiving gender medicine treatments continues to be unknown; (3) there is no reason to assume that the current generation of 5-25 year olds will NOT see 2% of their numbers experiencing these treatments.
New details that have arisen and will be discussed next: (1) the growth rate becomes unsustainable in 2023; (2) In the absence of further data (assumptions are provided), I recommend that the reader give these numbers a confidence of 50%, meaning the actual value is more likely than not between +-50%. Error bars are extremely difficult to reach with a paucity of data, and researchers require a budget to support this level of work. Every assumption made here would benefit from further research into its validity.
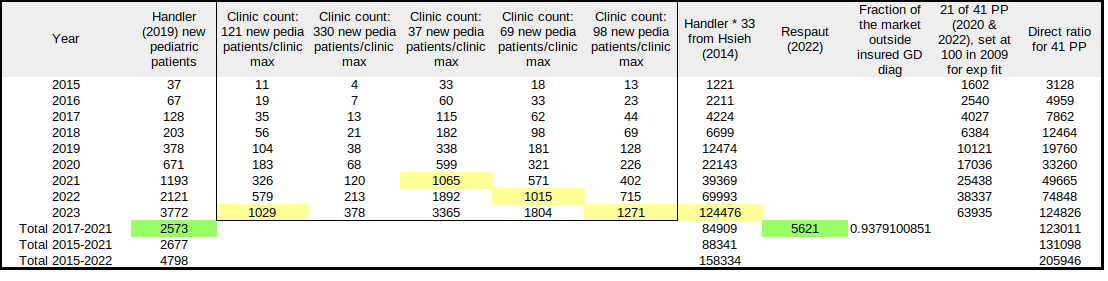
Table 1 assembles several papers of interest for comparison regarding the pediatric gender medicine population. To begin with, Handler et al (2019) provides details on the new patient population referred to a gender medicine clinic from 2015 to the first 6 months in 2018. 66% of the patients received treatments. The numbers shown in this table begin with "=ROUND('annual'*0.66)" until 2018 which is 2Xs that to complete the year. Then an exponential fit was performed, giving the equation "=ROUND(21.256*EXP(0.5754*('year'-2014)))". Note the '0.5754' growth function for comparison later.
The box within Table 1 provides information on the number of clinics. There are 4 data points to work with here. In 2014, Hsieh and Leininger listed the details of 33 pediatric gender med clinics in the US for "gender diverse" children to be treated. In 2021, the Society for Evidence-Based Gender Medicine estimated there were over 300, but no methodology was provided for reaching this number. The Gender Mapping Project counted over 400 in 2022 through the process of calling facilities that they identified through investigation and determining that they did in fact treat minors. Finally, a gender med nurse who gave witness testimony to the Missouri Attorney General, Jamie Reed, provided the detail that 604 new pediatric patients in 22 months at the clinic. This is around 330/year.
Assumption: this exponential growth and population size in Handler (2019) is applied across the 33 clinics from Hsieh (2014). The initial number in Handler indicates that a new clinic can be established with as few as 37 new patients/year. The number provided by Reed shows that a clinic can continue to handle as many as 330 patients/year. What the population growth is in any of the Hsieh clinics can vary significantly, but to get a first order estimate, we are applying the Handler numbers as being average.
The box within Table 1 begins with the population shown to the right of the box and calculates the number of clinics that would manage 121 new patients a year (every 3 days). As can be seen, in 2021 there are over 300 and in 2022 there are over 500. What is encouraging here relative to the assumption above is that the Gender Mapper estimate is a completely different data set. If we use it to test for an estimate of new patients driving the establishment of new clinics, we find that 330 new patients is too high and that less than 70 would be too small for the average (with the assumption above).
Regardless of which rate is selected, the establishment of over 1000 clinics, a jump of 400+ in a single year, would be noticeable in other information sources. There are no reports of such a large increase in facilities. Consequently, I perceive those numbers as being too high to be realistic. What that means is that the growth rate has become unsustainable. The year where that point is reached is 2022-2023 timeframe.
The next issue that needed to be addressed was Planned Parenthood, which handles a larger population than any of the gender med clinics, with the exception of an online clinic called Plume. Plume is for adults only, whereas Planned Parenthood will provide gender med treatments to minors (younger than 18 years old). A recent analysis of Planned Parenthood (PP) annual reports has been published in Brock and Anderson (2023). In it, they are able to determine two numbers of interest here: in 21 of 41 PP clinics, treatments were provided to a total of (a) 17,036 people in 2020 and (b) 38,337 people in 2022. Setting the initial population of people receiving these treatments in 2009 to 100, the exponential fit was "=(EXP(-921.139880739982+0.460803514659272*'year'))". The result of this calculation is shown in Table 1. Note that the exponential curve can have the same growth function, 0.57 as opposed to 0.46, if the initial population was 24-25 people.
Assumption test: I recommend calculating this growth rate, the variable product with time, for other data sets of pediatric gender med populations to compare.
Assumption: To estimate the total number of people receiving gender med treatments at Planned Parenthood, I then assumed that the numbers from the 21 annual reports were representative of the remaining, so I could divide the population by 21 and multiply by 41.
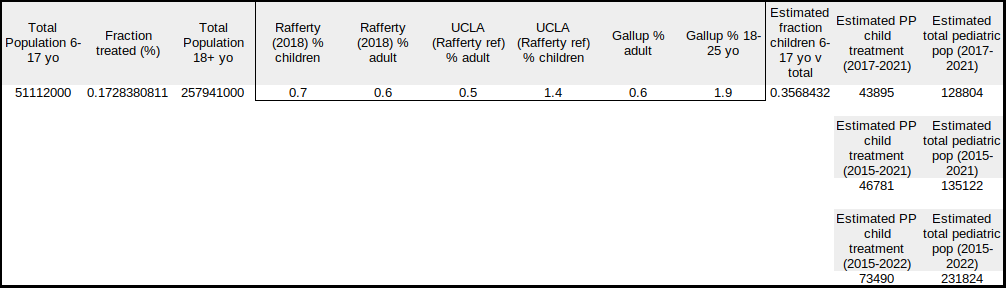
The next step to approximating the pediatric PP population was to estimate what the fraction of children to adults receiving gender med treatments was. There are multiple surveys with varying biases available. I looked at the Rafferty (2018) reference stating American Academy of Pediatrics policy, the more recent version of the UCLA survey cited in that paper, and a Gallup survey of young adults. There are also patient procedure numbers from hospitals relative to surgery, etc. There are issues and benefits to the information provided in all of these, and I would like to suggest a statistician take a close look. For now, I used the UCLA data as reported in the Tampa Bay Times to calculate: %children*totalchildren/(%children*totalchildren+%adults*totaladults)
where 'children' consists of 6-17 year olds for the calculation
This showed that roughly 0.356 or 36% of the PP population could be minors. A lot of assumptions went into this fraction, so be very careful using it.
In the final column of Table 2, I show the estimates for the total accumulating pediatric gender med population for the ranges of years shown. From the steepening growth in 2015 to 2022 when the growth becomes unsustainable, the total pediatric gender med population reaches 231,824. There are LARGE error bars on this calculation, but I am comfortable guessing that the actual number is more likely than not +-50% of this value.
From the steepening growth in 2015 to 2022 when the growth becomes unsustainable, the total pediatric gender med population reaches 231,824.
Issues that I have not discussed but which matter to this calculation include: (a) What is the ratio of trans-id'ing adults receiving gender med versus children? (b) What is the ratio of sterilization of trans-id'ing men versus women? What is the ratio of sterilization of trans-id'ing children versus adults? Puberty is crutial for fertility, but the larger pediatric cohort, teenage girls, are receiving gender med treatments later in puberty. Those who go no further than cross-sex hormones and double mastectomies could retain some fertility for example. (c) A number of US organizations and government institutions such as the American Academy of Pediatrics, the Endocrine Society, American Psychological Association, US Professional Association for Transgender Health, Health and Human Services, etc are legally involved in advocating for gender "affirming" medical treatments to be available to trans-id'ing children or "gender diverse" children. From this perspective, these numbers would indicate a significant demand for gender medicine exists and that the growth in facilities has yet to meet it.
To save my readers from having to scroll all the way to the bottom of this page, I'm adding these new references to the update. Until another researcher takes up this effort and performs a better quantitative analysis, this is likely the last update. Should that researcher not be me, I'll post a link above. Otherwise, the material you see here in this update is about to be submitted to a journal for peer review.
References in Update
Grace Abels (2023) "How many trans people are in the US — and why Americans often overestimate". PolitiFact article posted in Tamba Bay Times: https://www.tampabay.com/news/health/2023/07/13/politifact-how-many-people-are-transgender-estimates/
Note: This has the current UCLA and Gallup survey statistics shown in Table 2.
Megan Brock and Kate Anderson (2023) "Planned Parenthood’s Trans Hormone Business Is Booming, Creating Thousands of New Patients ‘For Life’". Daily Caller article posted in Ohio Star: https://theohiostar.com/news/planned-parenthoods-trans-hormone-business-is-booming-creating-thousands-of-new-patients-for-life/ohstarstaff/2023/12/20/
The Gender Mapping Project (2022). The South and Central American Gender Clinics and Their Patients. The Gender Mapping Project blog. https://www.gendermapper.org/post/the-south-and-central-american-gender-clinics-and-their-patients
Ted Handler, J. Carlo Hojilla, Reshma Varghese, Whitney Wellenstein, Derek D. Satre, Eve Zaritsky; Trends in Referrals to a Pediatric Transgender Clinic. Pediatrics November 2019; 144 (5): e20191368. https://doi.org/10.1542/peds.2019-1368
Sam Hsieh, BA and Jennifer Leininger, BA, BS. Resource List: Clinical Care Programs for Gender-Nonconforming Children and Adolescents. Pediatric Annals, 2014;43(6):238–244, DOI: https://doi.org/10.3928/00904481-20140522-11
Note: There were 33 in the US in 2014
Jason Rafferty, COMMITTEE ON PSYCHOSOCIAL ASPECTS OF CHILD AND FAMILY HEALTH, COMMITTEE ON ADOLESCENCE, SECTION ON LESBIAN, GAY, BISEXUAL, AND TRANSGENDER HEALTH AND WELLNESS, Michael Yogman, Rebecca Baum, Thresia B. Gambon, Arthur Lavin, Gerri Mattson, Lawrence Sagin Wissow, Cora Breuner, Elizabeth M. Alderman, Laura K. Grubb, Makia E. Powers, Krishna Upadhya, Stephenie B. Wallace, Lynn Hunt, Anne Teresa Gearhart, Christopher Harris, Kathryn Melland Lowe, Chadwick Taylor Rodgers, Ilana Michelle Sherer; Ensuring Comprehensive Care and Support for Transgender and Gender-Diverse Children and Adolescents. Pediatrics October 2018; 142 (4): e20182162. 10.1542/peds.2018-2162
Jamie Reed (2022) Genspect Denver Conference question and answer segment following Wilfred Reilly's presentation. https://youtu.be/if0FPZPqwX4?si=hcCWySlm6IojQ_yD&t=1986
Society for Evidence-Based Gender Medicine (2021). "Gender-affirming" Hormones and Surgeries for Gender-Dysphoric US Youth. Society for Evidence-Based Gender Medicine blog. https://segm.org/ease_of_obtaining_hormones_surgeries_GD_US
Update 7/18/2023: Thank you to everyone who has given me detailed feedback on this calculation! Additional sources of error and details on assumptions that are critical to the numbers shown are in this update with italics.
Update 7/22/2023: A worksheet question has been added to Ref A
Update 7/26/2023: A 3rd quality control data point is added to discussion at the end of this calculation.
For an upcoming publication, I was challenged to identify the size of the population of children receiving gender medicine treatments. As discussed below, between 1.83% and 7.95% of the USA's 6-17 year olds have received gender medicine treatments. A majority of them are expected to be sterilized. Finally, this population is projected to continue to grow significantly. AS ALWAYS, IT NEEDS TO BE ADDRESSED THAT THERE IS NO PROOF THAT GENDER MEDICINE REDUCES SUICIDE (Ref Ω).
Estimating the number of gender medicine patients in the US is challenging due to the diffuse nature of record-keeping. The following calculation proceeds as thus: (1) What is the size of the 6-17 year old population in the USA? (2) Of this population, how many are on Medicaid? (3) What is the size of the population in (2) that is receiving gender medicine treatments? (4) What is the ratio of non-medicaid patients receiving gender medicine to medicaid patients receiving gender medicine? (5) Using the ratio in (4), what is the Total population of gender medicine patients? (6) What percent of the total 6-17 year old population does this comprise? (7) What is the likelihood of this population being sterile from the treatments? Note that the alignment of the dates for the various data sets are offset from each other by one to three years; this introduces some error but not as much as Step 4.
Step 1 Census: The US Census has a range for the population size of 6-17 year olds in 2020 (Ref D). The middle series was selected as the error bars are greater in other areas of this calculation. The population size for this age group was 51,112,000.
Step 2 Medicaid proportion: One restriction that applies to this number is that Texas and Alabama did not permit medicaid funds to be used for gender medicine at the time the data was acquired in Reference A (Ref B). Arizona's medicaid population was also dropped in that no numbers were reported in the Reference for this (Ref C). So if we tally the total number of children on medicaid ages 0-17 years old, it is 36,774,810. Using the Census information for the total population of children ages 0-17 years old, we find that it is 74,660,000 children. The 6-17 year olds comprise 68.5% of the population (51,112,000/74,660,000*100). So the size of the population on medicaid (that can access gender medicine) that is 6-17 years old is 25,175,919.
Step 3 Percent of Medicaid 6-17 year olds Receiving Gender Medicine: The total of new medicaid patients aged 6-17 years between 2017 and 2021 was 121,872 (Ref A).
The Komodo report discussed in Reference A suffered from two problems (insofar as the Reuters reporting revealed): (1) It wasn't peer reviewed and isn't publicly available and (2) gender medicine commonly uses a legally-questionable approach called "creative coding" to bypass the codes used in the analysis. The text suggests that the analysis of the claims could not differentiate private and medicaid insurance claims without contacting individual states for medicaid information. I assume that this is due to some medicaid programs being delivered by private insurance companies. It also appears to have incomplete medicaid information, that not all states responded or were contacted. So given this issue, problem (2) "creative coding" was of particular concern. I'll leave the reader to research this particular topic, but the outcome is that gender medicine is provided without the codes that the Komodo report depended on. A suggested approach to estimate the size of this error would be for the analysts to identify specific gender providers and review the codes utilized for those patients receiving the treatments. The next issue is that given the legally-questionable environment for this type of insurance coding, how likely is it to be used for a medicaid patient as opposed to a private insurance patient. I'll leave the reader to look up how persistent healthcare fraud is in private insurance as opposed to medicaid. On top of this is the provision of medicaid by private insurers. The end result of these issues is that I set the number in this step to consist of all medicaid patients. I leave it to the reader to make modifications to this calculation. With respect to estimating errors, STEP 4 remains the greatest; however, the number from this STEP makes significant modifications to those error bars. While many of the errors are not iterative, this STEP and STEP4 are cumulative and must be evaluated carefully. See my comments at the end of this article for a potential independent check on this approach.
The fraction that this comprises is 121,872/25,175,919=0.00484 which is 0.484%. NOTE THAT THIS IS THE NEW PATIENT POPULATION. We don't know what it initially started out at, so that would make the total population size larger. We also do not have a good measure of the loss rate as children change their minds (see Ref K), but one study showed it to be very low (Ref E, note population problems in the SEGM link following the reference). These are additional sources of error but they are very small relative to the other sources.
Step 4 is the Ratio of Non-Medicaid Patients to Medicaid Patients: This is the greatest source of error in the calculation of pediatric gender medicine population size (irrespective of fertility status). In Reference E, the incomes of the participants in a five-year long study on the pediatric gender medicine population was conducted. By the end of the study, 60% of the children were receiving gender medicine treatments. The income breakdown by percent was 3% had incomes less than $25k and 10% had incomes greater than $25k but less than $50k. Among the 60% of children treated, how many would have qualified for medicaid? Anecdotally, a number of doctors and nurses have reported on how few lower income pediatric gender medicine patients there are. Another study allows a potential examination; it documents that 70 out of 4,118 adult gender medicine patients were on medicaid or 1.7% (Ref F). Therefore we could assume that anywhere between 3% to 13% of the participants in the study could access gender medicine on medicaid. The lower this %, then the larger the % of the population is being sterilized, as will become apparent.
Step 5 Total Pediatric Gender Medicine Population: This is a basic calculation where
fraction_non-medicaid*Total + fraction_medicaid*Total = Total
and we know
fraction_medicaid*Total = 121,872
so
Total = 121,872/fraction_medicaid = 121,872/[0.03 , 0.13]
Notice that []'s show the two options from Step 4. So we then find
Total = [4,062,400 , 937,477]
for the 3% and 13% medicaid participants respectively.
Step 6 Percent that the Total Gender Medicine Population Comprises of the Whole: The calculation for this is as follows
[4,062,400 , 937,477]/51,112,000 = [0.0795 , 0.0183]
which is 7.95% and 1.83% respectively. Recall that earlier we calculated the % of the population accessing medicaid that received gender medicine treatments at 0.484%. It is informative to calculate the percent of the 6-17 year old population that cannot access medicaid receiving these treatments.
[(4,062,400-121,872)/(51,112,000-25,175,919) , (937,477-121,872)/(51,112,000-25,175,919)] = [0.152 , 0.041]
which is 15.2% and 4.1% of this non-medicaid total population.
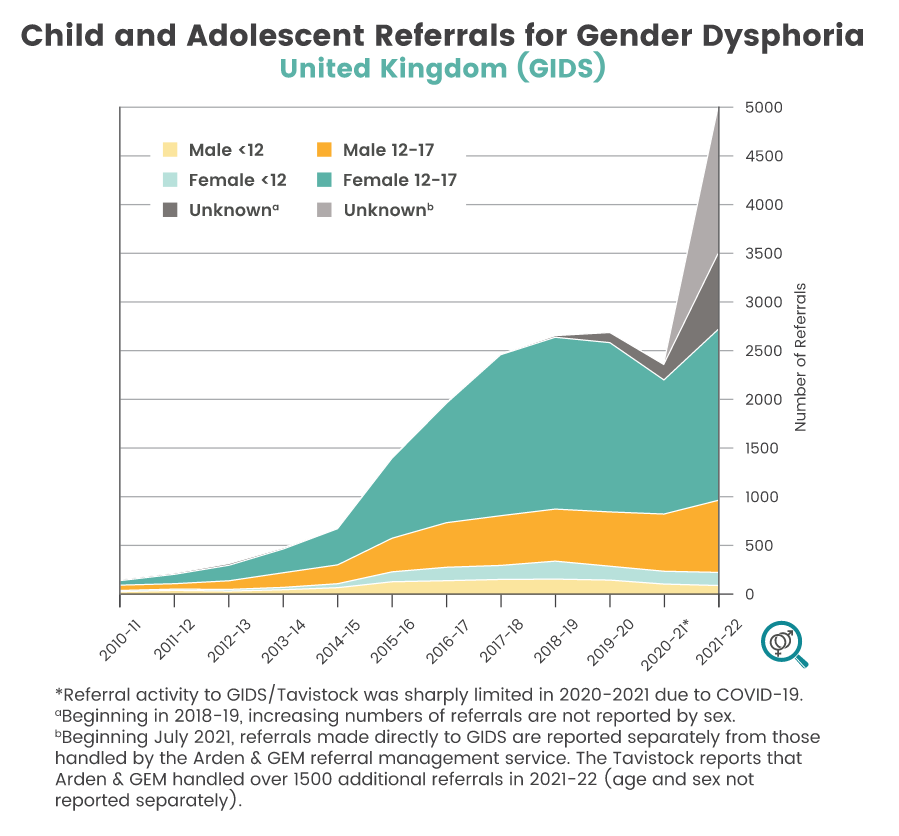
Note that this number is not stable, rather it's growing at an exponential rate. The plot in Ref A is similar to a UK gender service new patient reference population with time showing an exponential increase in the population seeking gender medicine. This has been observed in multiple countries.
Step 7 Fertility Damage (Sterility):
There are no solid studies measuring the impact of pediatric gender medicine on fertility/sterility, but it is apparent that this is an issue of significant concern. Various sources are compiled here for the reader to pursue.
1) On surgical gender medicine: "hysterectomy and oophorectomy in transmen or orchiectomy in transwomen results in permanent sterility" (Ref H). The latest guidelines from The World Professional Association of Transgender Health (WPATH) Standards of Care have eliminated age recommendations except for the phalloplasty procedure which would follow the hysterectomy (Ref J). While some children have had this treatment, it is rare until they reach age 18 years old when it becomes more common.
2) On puberty blockers followed by cross-sex hormones: "Suppression of puberty with gonadotropin-releasing hormone agonist analogs (GnRHa) in the pediatric transgender patient can pause the maturation of germ cells, and thus, affect fertility potential. Testosterone therapy in transgender men can suppress ovulation and alter ovarian histology, while estrogen therapy in transgender women can lead to impaired spermatogenesis and testicular atrophy. The effect of hormone therapy on fertility is potentially reversible, but the extent is unclear. " See Ref H's research article link.
4) The concern over fertility/sterility is of such magnitude that gender medicine practitioners discuss experimenting with preserving fertility and attempting strategies such as having children write to their future selves that they don't want children (Reference I).
Simple Question
Simple question: how many kids are getting sterilizing hormones/puberty blockers/surgery? As shown above, finding the answer to this is quite complicated. On twitter, Leor Sapir went and invited me to "inspect the underside of a bus carriage" as one of my followers phrased it. He never contacted me prior to reacting to this calculation. Another twitterer claiming to be an academic suggested that readers are not mature enough to deal with this material and plans to write a letter demanding this academic endeavor be silenced (the opposite of academic freedom). Here an important point: no one's questioning the math. Sapir is reacting with concern that if the numbers shown are way off, then politically it could be used against the effort to push back on the ethics of gender medicine. Data is data, and while this article's title could be a little less sensationalized, I am being far more open in identifying and discussing unknowns and errors than the vast majority of researchers in the gender medicine field, particularly Tordoff. I'm carefully evaluating each piece of information that is presented, acknowledging the issues in the calculation, and presenting this to my reader under the assumption that a mature adult deserves to be treated like a mature adult. For example, let's say you the reader decides that the legally-questionable coding issue isn't as problematic as I assumed in STEP 3 and reduce the number by 1/2, which will bring the calculation down to around 0.9%-4%. Regardless, the final point I made is still there: exponential growth. I may be overestimating right now, but not for long.
Testing
One detail which I didn't mention when this was initially posted is that the lower boundary condition for the solution space landed right on top of the responses from a Gallup survey of Gen Z adults: 1.9%
https://www.tampabay.com/news/health/2023/07/13/politifact-how-many-people-are-transgender-estimates/
[*deleted text at bottom, note correction from 'parents'; finally had time to read the survey report linked through the article.]
Update July 21, 2023: I am currently in a back and forth discussion on the errors in these various references, and we seem to be coming to a conclusion on where the remaining issues are. It is important to note that I'm making the following assumptions in the calculations: (a) a gender dysphoria diagnosis accompanies social transitioning, (b) social transitioning is almost guaranteed to become medical transitioning for all children (not adults, unless they socially transitioned as children). Now further checks on the numbers are as follows.
Ground truth: you the reader, look around you and think of how many children you know well enough to know if they are/aren't receiving gender med treatments; then calculate what is the ratio of those who are being treated to the total?
Next, in the National College Health Assessment for undergraduates, it appears that 6% of those who answered the question identify as transgender/GNC (https://www.acha.org/documents/ncha/NCHA-III_FALL_2022_UNDERGRADUATE_REFERENCE_GROUP_EXECUTIVE_SUMMARY.pdf). It's not explicitly stated; however, given the members conducting the survey, it appears that this is among the population seeking campus health services. If that assumption is correct, then my calculation above for this non-medicaid population would be at least 4.1%.
So next lets do a is-it-physically-possible check. According to SEGM, over 300 gender clinics are estimated to be providing pediatric care in the US (https://segm.org/ease_of_obtaining_hormones_surgeries_GD_US). Planned Parenthood sets the minimum age for services at 16 years and operates 41 of these alone (including telehealth), for example. Lets take the lower boundary from the calculation above: 930,000 over 5 years. So, that would make each clinic seeing 3,100 new patients on average over the 5 cumulative years. If we weight the later years due to exponential growth and say half of those appeared in the last two years, that would be 775 new patients each year at each clinic or 65 new patients each month. Especially given Planned Parenthood has a major role in all this, do the numbers look impossible? A paper published in 2019 gives insight into a pediatric gender clinic that is not Planned Parenthood (Ref L). In it, the authors state, "Average monthly referrals increased from 5.1 in 2015 to 25.7 in 2018, an increase of 504%." To take the calculation in this paragraph and see what it would predict for 2018, it proceeds as thus: 930,000 new_patients/5 years/300 clinics = 3,100 new_patients/clinic/5 years -> to incorporate exponential growth, this was divided as 1,550 new_patients/3 years/clinic (2017-2019) + 1,500 new_patients/2 years/clinic (2020-2021), the latter part has been already calculated for 2020-2021 -> the former part comes to 516 new_patients/year/clinic for 2017-2019, which is 43 new_patients/month/clinic. This calculated rate is 43/25.7 = 1.7 times larger than the reported population in the paper. Given the error bars involved in my calculation, this is quite close. The paper's 25.7 new_patients/month/1 clinic is significantly below the lowest value in the calculation, making it a potential modifier to the STEP3 assumptions, and it is an excellent data point for reliability; however, until the Planned Parenthood numbers come in for how they impact the average, it is not clear how to extrapolate on this single clinic.
I'll leave it to you, the reader, to look up market reports on the projected growth of profits from this population; also take a look at announcements for new clinics providing services or established practices broadening services to include gender med. Then consider what that means relative to the numbers provided herein.
[*deleted: "Again, this is a squishy number in that it suffers from standard surveying problems and how many of the parents saying their kids are trans are also going for the gender dysphoria diagnosis? It's more likely than not in my opinion, and the bias of liberals (who are more likely to have trans id'ing children) to answer surveys over conservatives suggests the number may be somewhat useful."]
Ref Ω) Jensen, E.A. (2022) "Medical Safety: Risk Study of Gender Medicine, Part 2." Website: https://4w.pub/medical-safety-risk-study-of-gender-medicine-part-2/
Jackson D (March 20, 2023) "Suicide-Related Outcomes Following Gender-Affirming Treatment: A Review." Cureus 15(3): e36425. https://doi.org/10.7759/cureus.36425
Ref A) R. Respaut and C. Terhune (Oct. 6, 2022) "Putting numbers on the rise in children seeking gender care." Reuters News. https://www.reuters.com/investigates/special-report/usa-transyouth-data/
Worksheet question: Take a look at the Figure titled, "Diagnoses among Medicaid patients in selected states". Plot 2020 Medicaid numbers against state population sizes. Notice a problem?
Ref B) I. Gomez et al. (Oct 11, 2022) "Update on Medicaid Coverage of Gender-Affirming Health Services." Website: https://www.kff.org/womens-health-policy/issue-brief/update-on-medicaid-coverage-of-gender-affirming-health-services/
Ref C) Medicaid.gov (2023) "January 2023 Medicaid & CHIP Enrollment Data Highlights." Website: https://www.medicaid.gov/medicaid/program-information/medicaid-and-chip-enrollment-data/report-highlights/index.html
Ref D) US Census Bureau (2020) "National Demographic Analysis Tables: 2020." Website: https://www.census.gov/data/tables/2020/demo/popest/2020-demographic-analysis-tables.html
Ref E) Kristina R. Olson, Lily Durwood, Rachel Horton, Natalie M. Gallagher, Aaron Devor; Gender Identity 5 Years After Social Transition. Pediatrics August 2022; 150 (2): e2021056082. https://doi.org/10.1542/peds.2021-056082
Note population issues with the article discussed in: https://segm.org/early-social-gender-transition-persistence
Ref F) Canner JK, Harfouch O, Kodadek LM, et al. Temporal Trends in Gender-Affirming Surgery Among Transgender Patients in the United States. JAMA Surg. 2018;153(7):609–616. https://doi.org/10.1001/jamasurg.2017.6231
Ref G) Society for Evidence Based Gender Medicine, Website: https://segm.org/
Ref H) Stats for Gender, Website with links to research articles: https://statsforgender.org/fertility/
Ref I) Denise (2021) "TMI: Genderqueer 11-year-olds can’t handle too much info about sterilizing treatments–but do get on with those treatments." Website with links to original data (gender medicine practitioner presentation materials): https://4thwavenow.com/2021/04/13/tmi-genderqueer-11-year-olds-cant-handle-too-much-info-about-sterilizing-treatments-but-do-get-on-with-those-treatments/
Ref J) E. Coleman, A. E. Radix, W. P. Bouman, G. R. Brown, A. L. C. de Vries, M. B. Deutsch, R. Ettner, L. Fraser, M. Goodman, J. Green, A. B. Hancock, T. W. Johnson, D. H. Karasic, G. A. Knudson, S. F. Leibowitz, H. F. L. Meyer-Bahlburg, S. J. Monstrey, J. Motmans, L. Nahata, T. O. Nieder, S. L. Reisner, C. Richards, L. S. Schechter, V. Tangpricha, A. C. Tishelman, M. A. A. Van Trotsenburg, S. Winter, K. Ducheny, N. J. Adams, T. M. Adrián, L. R. Allen, D. Azul, H. Bagga, K. Başar, D. S. Bathory, J. J. Belinky, D. R. Berg, J. U. Berli, R. O. Bluebond-Langner, M.-B. Bouman, M. L. Bowers, P. J. Brassard, J. Byrne, L. Capitán, C. J. Cargill, J. M. Carswell, S. C. Chang, G. Chelvakumar, T. Corneil, K. B. Dalke, G. De Cuypere, E. de Vries, M. Den Heijer, A. H. Devor, C. Dhejne, A. D’Marco, E. K. Edmiston, L. Edwards-Leeper, R. Ehrbar, D. Ehrensaft, J. Eisfeld, E. Elaut, L. Erickson-Schroth, J. L. Feldman, A. D. Fisher, M. M. Garcia, L. Gijs, S. E. Green, B. P. Hall, T. L. D. Hardy, M. S. Irwig, L. A. Jacobs, A. C. Janssen, K. Johnson, D. T. Klink, B. P. C. Kreukels, L. E. Kuper, E. J. Kvach, M. A. Malouf, R. Massey, T. Mazur, C. McLachlan, S. D. Morrison, S. W. Mosser, P. M. Neira, U. Nygren, J. M. Oates, J. Obedin-Maliver, G. Pagkalos, J. Patton, N. Phanuphak, K. Rachlin, T. Reed, G. N. Rider, J. Ristori, S. Robbins-Cherry, S. A. Roberts, K. A. Rodriguez-Wallberg, S. M. Rosenthal, K. Sabir, J. D. Safer, A. I. Scheim, L. J. Seal, T. J. Sehoole, K. Spencer, C. St. Amand, T. D. Steensma, J. F. Strang, G. B. Taylor, K. Tilleman, G. G. T’Sjoen, L. N. Vala, N. M. Van Mello, J. F. Veale, J. A. Vencill, B. Vincent, L. M. Wesp, M. A. West & J. Arcelus (2022) Standards of Care for the Health of Transgender and Gender Diverse People, Version 8, International Journal of Transgender Health, 23:sup1, S1-S259, DOI: 10.1080/26895269.2022.2100644
Ref K) Roberts CM, Klein DA, Adirim TA, Schvey NA, Hisle-Gorman E. Continuation of Gender-affirming Hormones Among Transgender Adolescents and Adults. J Clin Endocrinol Metab. 2022 Aug 18;107(9):e3937-e3943. doi: 10.1210/clinem/dgac251. PMID: 35452119. https://pubmed.ncbi.nlm.nih.gov/35452119/
Ref L) Ted Handler, J. Carlo Hojilla, Reshma Varghese, Whitney Wellenstein, Derek D. Satre, Eve Zaritsky; Trends in Referrals to a Pediatric Transgender Clinic. Pediatrics November 2019; 144 (5): e20191368. 10.1542/peds.2019-1368 https://publications.aap.org/pediatrics/article/144/5/e20191368/38227/Trends-in-Referrals-to-a-Pediatric-Transgender
Enter your email below to sign in or become a 4W member and join the conversation.
(Already did this? Try refreshing the page!)


Comments